Anterior chest wall involvement in SAPHO syndrome



Clinical History
A 55-year-old woman presented with general arthralgia and axial pain since many years. Clinical inspection revealed palmoplantar pustulosis.
Imaging Findings
Chest radiography showed sclerosis of the medial aspect of the left clavicle (Figure 2).
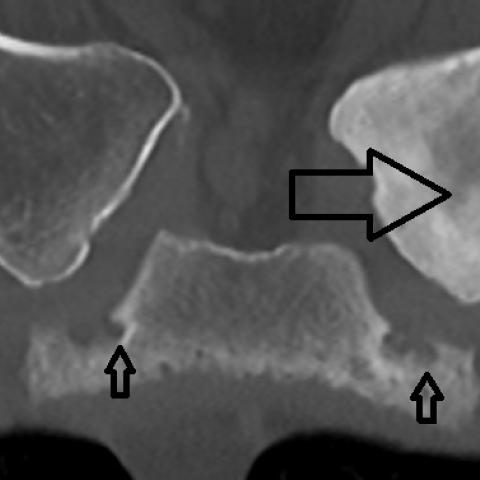
CT confirmed osteosclerosis and periosteal reaction at the left clavicle. Erosions were seen at the sternoclavicular and costosternal joints with ligamentous ossification of the left costoclavicular ligament (Figure 3a-b).
MRI of the sternoclavicular joints revealed a mixture of sclerosis and bone marrow oedema (Figure 4a-c). After administration of gadolinium contrast, there was also enhancement of the left clavicle (Figure 4d).
Discussion
SAPHO is an acronym that stands for synovitis, acne, pustulosis, hyperostosis and osteitis.
The hallmark of the skin manifestations is palmoplantar pustulosis and acne [1].
SAPHO syndrome tends to involve the axial skeleton and the anterior chest wall, especially the sternoclavicular joint, with clavicular involvement typically starting at the medial aspect [2]. Spinal involvement is usually monovertebral, with the thoracic spine being most frequently affected [3]. Sacroiliitis is also sometimes seen. Peripheral joints in the form of a mono- or polyarthritis can also be affected, but to a lesser extent [4].
Its pathogenesis is still not completely understood. There is an association with HLA-B27 and different pathogens were isolated from different bone sites and pustules in the skin. The most probable hypothesis is that it is caused by autoimmune reactions in genetically predisposed individuals triggered by some infectious agent [5].
Patients present with pain, swelling, and limitation of movement, most often in the anterior chest wall. In many patients, there is a considerable delay in the correct diagnosis [1].
In children and adolescents, a similar condition called chronic recurrent multifocal osteomyelitis (CRMO), more commonly involves the long bone metaphyses and clavicles [1].
The imaging features are dominated by hyperostosis, osteitis and synovitis, arthritis, and chronic inflammatory bone disease. Osteitis consists of inflammation of the medullary bone, which manifests as osteosclerosis on conventional radiography. The term hyperostosis is used to designate chronic periosteal reaction and cortical thickening leading to bone hypertrophy. Radiography is usually the initial modality and can reveal sclerosis and periosteal reaction in advanced disease, but it is less sensitive for early detection. CT scan is the preferred modality to demonstrate osteosclerosis and/or hyperostosis, erosions, and ligamentous ossifications. MR imaging on the other hand, is best suited for demonstration of inflammatory changes and bone marrow oedema using fluid-sensitive sequences. Whole-body MRI is recommended for the evaluation of multifocality and asymptomatic lesions [6, 7].
The treatment remains a challenge. It includes administration of nonsteroidal anti-inflammatory drugs, corticosteroids, methotrexate, and tumour necrosis factor alfa inhibitors. Except for a minority of patients who have a self-limited course, most of them have either a relapsing-remitting course or a chronic indolent disease pattern [5].
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
SAPHO syndrome with anterior chest wall involvement
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures








I. Radiographic Findings
Based on the X-ray, CT, and MRI images provided by the patient, the following main features can be observed:
1. Sternoclavicular Joint: X-ray and CT indicate proliferative or reactive sclerosis around the sternoclavicular joint, with some irregular margins or mild erosive changes, consistent with chronic osteitis or hyperostosis.
2. Sacroiliac Joint: CT and MRI show changes in bone density of the articular surfaces and inflammatory infiltration; on T2WI or other fluid-sensitive sequences, bone marrow edema and infiltration signals are visible, suggesting chronic inflammatory changes in the joint and surrounding bone tissue.
3. Skin Manifestations: Photos of the patient’s palms and soles reveal multiple small pustules and pigmentation marks, consistent with the typical presentation of palmoplantar pustulosis.
4. Others: No obvious signs of acute fracture are seen; no large-scale significant swelling or fluid accumulation in the surrounding soft tissue. Radiographic signs of chronic inflammatory processes (such as abnormal bone marrow signals and cortical thickening) are noted.
II. Possible Diagnoses
Based on the patient’s clinical presentation (palmoplantar pustulosis, long-standing axial skeletal pain) and the above radiographic findings, the following diagnoses are primarily considered:
1. SAPHO Syndrome: SAPHO consists of synovitis, acne, pustulosis, hyperostosis, and osteitis, commonly involving the sternoclavicular joint, clavicle, and sacroiliac joints, with palmoplantar pustulosis as a typical skin manifestation. On imaging, hyperostosis, bone marrow edema, and chronic inflammatory changes are frequently observed.
2. Psoriatic Arthritis: This may present with skin lesions (including pustular psoriasis), affecting peripheral joints and the axial skeleton. Radiographically, it can also show joint inflammation and bone changes, but it more commonly involves the distal interphalangeal joints of the hands and feet, as well as the spine; sternoclavicular joint involvement is relatively less common.
3. Chronic Infectious Arthritis/Osteomyelitis: Infectious factors can lead to chronic osteomyelitis and bony changes, but typically show more significant local destruction and soft tissue abscess (with obvious bone destruction, sequestra, or soft tissue abscess cavity on imaging). Based on the current imaging and medical history, this possibility is lower.
III. Final Diagnosis
Considering the patient’s longstanding axial skeletal pain, the typical skin manifestations of palmoplantar pustulosis, and chronic inflammatory and hyperostotic changes in the sternoclavicular and sacroiliac joints on imaging, the most likely diagnosis is:
SAPHO Syndrome.
Further confirmation could involve serologic tests (inflammatory markers, ruling out infection) as well as skin biopsy or additional imaging follow-up. If clinical suspicion is high, combined with existing imaging features and typical skin manifestations, SAPHO Syndrome is relatively clearly indicated.
IV. Treatment Plan & Rehabilitation
Treatment Strategies:
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Often used as first-line therapy to alleviate joint and bone pain and reduce inflammation.
2. Corticosteroids: Short-term use during periods of significant active inflammation can rapidly relieve symptoms.
3. Disease-Modifying Antirheumatic Drugs (DMARDs): Such as methotrexate (MTX) to control chronic inflammation and prevent bone and joint damage.
4. Biologics: For instance, TNF-α inhibitors may be considered for patients who do not respond well to conventional therapy.
5. Management of Skin Lesions: Coordinate with dermatologists for topical or oral medications to improve palmoplantar pustulosis and reduce discomfort.
Rehabilitation and Exercise Prescription:
1. General Principle: For chronic bone and joint conditions, exercise within the tolerable range of pain should be performed progressively to avoid disuse atrophy and maintain joint flexibility.
2. Type of Exercise: Low-impact exercises are recommended initially, such as gentle range-of-motion exercises (for the shoulder joints, thorax, hip joints, etc.), swimming, or water aerobics, which place less stress on the joints.
3. FITT-VP Principle:
· Frequency: 3–5 sessions per week, depending on symptoms and physical capacity;
· Intensity: Start at a low intensity (for example, maintaining heart rate at 50–60% of the maximum) and increase gradually;
· Time: 20–30 minutes per session, possibly divided into segments according to tolerance;
· Type: A combination of low-impact aerobic exercises and joint flexibility training, with strength training (light resistance, resistance bands, etc.) as needed;
· Progression: Reassess exercise tolerance and joint function every 2–4 weeks, and make small adjustments to intensity or duration as appropriate;
· Volume: Aim to gradually increase total weekly exercise volume.
4. Special Considerations:
· Patients with sternoclavicular joint or spinal pain should avoid excessive loading or large twisting movements;
· Beware of increased pain from sustained high-load activities. If significant discomfort or joint inflammation occurs, rest and timely re-evaluation are necessary.
V. Disclaimer
This report is based on the current clinical and radiological information for analysis and is for medical reference only. It does not replace an in-person consultation or the final judgment and treatment advice of a medical professional. Patients should tailor and adjust their treatment and rehabilitation plans under the guidance of qualified healthcare providers, taking into account their individual circumstances.
Human Doctor Final Diagnosis
SAPHO syndrome with anterior chest wall involvement