


The imaging features are described of a 15 year old male presenting with pain in the lower leg . Radiographs and CT showed a well-defined metaphyseal lucency abutting the physis . MR imaging also demonstrated extensive bone marrow oedema.
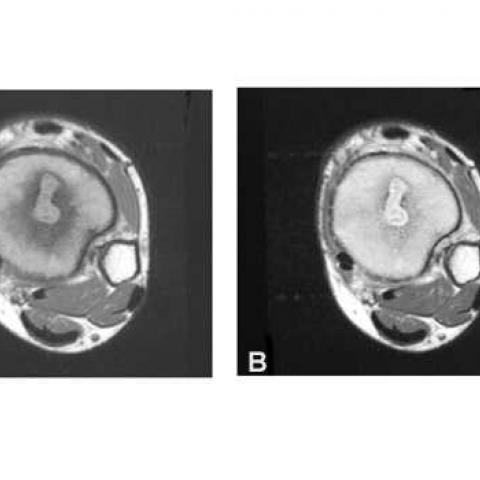
A 15 year old male presented with a 3 month history of pain in his left lower leg . On examination there was tenderness and slight swelling over the distal tibia . He was afebrile . Radiographs showed a well-defined , flame-shaped lucency in the distal tibial metaphysis surrounded by considerable sclerosis (Fig. 1) . Infection was suspected and technetium99 methyldiphosphonate (MDP) scintigraphy performed .This demonstrated markedly increased uptake on all three phases in the distal tibia only (Fig. 2). CT confirmed the presence of a well-defined lucency with surrounding sclerosis in the metaphysis and reformatted images showed its precise relationship to the growth plate (Fig. 3a,b) .A small sequestrum was also demonstrated (Fig. 3c). Magnetic resonance (MR) imaging clearly demonstrated the full extent of the cavity and showed extensive soft tissue changes in the bone marrow which extended into the epiphysis (Fig. 4). Following intravenous gadolinium-DTPA there was marked enhancement of both the margins of the cavity and surrounding soft tissues .There was no joint effusion and only minor changes in the extra-osseous soft tissues . The cavity was surgically drained under general anaesthesia and culture showed staphylococcus aureus . Recovery was uneventful .
Osteomyelitis is usually due to haematogenous spread of infection to bone . Commonest in children and young adults , the metaphysis of a long bone is usually affected reflecting its rich blood supply . The tibia is the commonest site affected (1). In the immature skeleton the physeal plate acts as a barrier preventing the spread of infection to the epiphysis . In infants , blood vessels penetrate the physis (growth plate) allowing infection to extend into or primarily affect the epiphysis (2). An intraosseous or Brodie`s abscess is a complication of subacute osteomyelitis and typically is seen on radiographs as a central , well-defined metaphyseal lucency with surronding reactive sclerosis . The presence of a channel or tract connecting this lucency to the physis is characteristic (3). Cortical extension results in periostitis and involvement of the extra-osseous soft-tissues . Technetium 99 MDP scintigraphy demonstrates intense uptake on flow,diffusion and delayed images and is particularly useful in excluding other areas of clinically occult infection . CT more clearly defines the margins of the abscess cavity, the extent of soft tissue involvement and is very sensitive in identifying sequestra .Rarely fat-fluid levels and gas are also demonstrated within the abscess . On MR imaging Brodie`s abscesses appear as well-defined intra-osseous regions of low-to-intermediate signal intensity on T1-weighted images and of high signal intensity on T2-weighted images surrounded by a rim of low signal intensity due to sclerotic bone (4).They are surrounded by extensive changes in the bone marrow which may extend into the extra-osseous soft tissues . The differentiation of soft tissue extension of infection and soft tissue oedema , however , is difficult . Following intravenous gadolinium these soft tissue changes and granulation tissue lining the abscess cavity and associated tracks enhance . Sequestra appear as areas of low signal on all sequences and do not enhance . Although MR imaging is the most sensitive method of diagnosing musculoskeletal infection, it remains non-specific despite the description of several helpful ancillary signs (5).The differential diagnosis of Brodie`s abscess includes bone neoplasms including , particularly when small and cortically located , osteoid osteomas .
Brodie`s Abscess







1. X-ray and CT findings: There is a well-defined lucent area in the distal tibial metaphysis, surrounded by sclerotic reaction. The lesion is observed to be connected to the epiphyseal plate, forming a channel-like structure, which to some extent suggests an infectious lesion or abscess.
2. MRI findings: The lesion appears low to intermediate signal on T1-weighted images and hyperintense on T2-weighted images, with significant bone marrow edema around the lesion. Soft tissue edema or inflammatory changes are also noted. After contrast administration, the lesion wall and surrounding soft tissue show obvious enhancement, consistent with inflammatory exudation or granulation tissue proliferation.
3. Isotope bone scan: Significant tracer uptake is detected at the site of pain, supporting the presence of active inflammation.
1. Subacute Osteomyelitis (Brodie’s abscess): Based on the patient’s adolescent age, the location of the lesion in the tibial metaphysis, radiographic findings of a lucent area surrounded by sclerosis, and extensive bone marrow and soft tissue edema. The typical channel or tract connecting to the epiphyseal plate is also a common feature of Brodie’s abscess.
2. Bone tumors (e.g., osteoid osteoma): When the lesion is located in the cortical bone, especially if it presents as a relatively small and well-defined radiolucent nidus, benign bone tumors such as osteoid osteoma should be considered. However, in this case, the imaging features are more suggestive of an infectious process (marked bone marrow edema, sclerotic margin, and tract formation).
Combining the patient’s age, clinical symptoms (pain in the distal tibia), and imaging findings (a focal lucent area with a sclerotic rim and enhancement in the metaphysis, along with bone marrow and soft tissue edema), the most likely diagnosis is:
Subacute Osteomyelitis (Brodie’s abscess).
1. Pharmacotherapy and Other Conservative Treatments:
• Select appropriate antibiotics targeting common pathogens (such as Staphylococcus aureus), administered intravenously or orally. The treatment duration is usually long (lasting weeks to months), depending on clinical and imaging follow-up findings.
• Surgical intervention: In cases with a larger lesion, significant symptoms, or lack of improvement with medical treatment, curettage of the lesion may be considered, possibly with the placement of antibiotic-impregnated cement to clear the abscess cavity and prevent recurrence.
2. Rehabilitation/Exercise Prescription Suggestions (FITT-VP Principle):
• Phase 1 (Acute Inflammation Control): Primarily reduce weight-bearing and limit activity; use assistive devices or crutches to avoid excessive loading on the affected bone. Training focuses on simple range-of-motion exercises and isometric muscle contractions. The frequency can be 1–2 times a day, each session 5–10 minutes, mainly to prevent muscle atrophy and joint stiffness.
• Phase 2 (Symptom Relief/Stabilization): After anti-infective treatment has achieved some effect and pain is reduced, gradually increase lower limb functional exercises, such as low-intensity ankle and knee flexion/extension and core strength training under the guidance of a physical therapist. The frequency can be 3–4 times a week, each session 20–30 minutes, with an intensity that does not cause pain or discomfort.
• Phase 3 (Recovery): Once imaging and clinical symptoms show significant improvement, progressively introduce weight-bearing exercise, such as standing balance training and short-distance walking exercises. If conditions allow, gradually transition to low-impact aerobic activities (swimming, cycling, etc.). The frequency can be 3–5 times a week, about 30 minutes each time, ensuring proper form and safety.
• Phase 4 (Advanced Exercise Stage): Upon follow-up confirmation of lesion healing and stable bone structure—based on the patient’s muscle strength and bone health—gradually add light jogging, mild jumping, etc., combined with core stability and flexibility training. Perform these exercises 3–4 times a week, for 30–45 minutes per session, progressively increasing intensity.
• Notes: Throughout the rehabilitation process, regular follow-up imaging and blood tests are needed. If any discomfort or worsening pain occurs, seek medical attention promptly and adjust the rehabilitation plan. For patients with relatively fragile bones or other underlying conditions, load-bearing and exercise intensity should be more cautiously regulated to avoid fractures or other complications.
This report only provides a reference analysis based on the available imaging and clinical information and cannot replace an in-person consultation or professional medical advice. If you have further questions or changes in your condition, please consult a specialist or visit a qualified medical institution.
Brodie`s Abscess