Rectus femoris muscle tear



Clinical History
A 7 year-old male refers mild pain in the anterior compartment of the thigh for 1 month without an inciting traumatic event. The patient has not experienced sudden acute pain at any time. The physical exam reveals a palpable 3x8-cm anterior thigh mass of soft tissue consistency.
Imaging Findings
The patient is a 7 year-old male with mild pain in the anterior compartment of the thigh for 1 month. There is a non-specific history of an inciting traumatic event and the patient has not experienced sudden acute pain at any time. The physical exam reveals a palpable 3x8-cm anterior thigh mass of soft tissue consistency. The mass appears to be within the substance of the rectus femoris muscle. The affected thigh is asymmetric as compared with the contralateral one. There is no functional deficit. Vascular and neurological examination of the affected limb is normal. Laboratory data without relevant findings. Ultrasonography and MRI are performed.
Discussion
The quadriceps muscle, considered as a muscle group functioning over two joints and undergoing eccentric contraction, is at increased risk of injury in contact and strenuous sports. Strain injuries of this muscle are common and may appear with a triad of localized swelling and increased thigh circumference, thigh pain and loss of knee flexion [1]. A rectus femoris muscle tear, as a type of quadriceps muscle strains, in itself, may not cause a significant or measurable functional deficit. After an acute injury the knee flexion is limited and painful. However, a chronic tear may appear as a mass without functional deficit or pain. In both, acute and delayed-onset muscle lesions, Ultrasound and MR imaging may provide information not available at physical examination, localizing tissue abnormalities, confirming the presence or absence of focal hematoma and showing no evidence of fatty infiltration or fibrosis. The T2-weighted scans show the lesion as a focus of abnormal high intensity signal in the muscle surrounding the tendon. Another pattern on T2-weighted images consists of the tendency for MR abnormalities to occur in concentric zones, with perifascial "rim sign", explained by haemorrhage or edema from muscle necrosis. A central circular and high intensity area is noted, probably due to an intramuscular fluid collection, surrounded by a concentric low intensity ring, and peripheral high intensity rim [2]. Fibrotic tissue usually results in areas of low signal intensity in all sequences. The use of gadolinium-enhanced T1 weighted MRI is very useful for accentuating the lesion. The T1-weighted images after intravenous gadolinium may enhance the muscular component, with the appearance of a "bull's eye", with an enhancing mass centred about a hypo-intense structure corresponding to the intramuscular tendon [3]. The uptake of gadolinium in the area of the muscle injury is due to the increased vascularity of the lesion. Sonographic findings in muscular ruptures include direct and indirect signs such as the discontinuity of muscle fibers and the presence of an associated hematoma. In complete ruptures, sonograms show the "clapper-in-the-bell" sign. However, identifying the torn fragments of the injured muscle may be difficult. Real-time examination during contraction better demonstrates the gap between the muscle fragments. On sonograms of partial ruptures, the injured area shows jagged margins, and a surrounding hyper-echoic halo may be present. A clapper-in-the-bell sign can also be present and is pathognomonic of a rupture. A combination of longitudinal and transverse sonograms is required to determine the exact size and location of a rupture. Our patient underwent MRI evaluation, which showed, as the physical examination, a mass at the rectus femoris muscle. A tissue biopsy was performed, with the result of chronic inflammation and reactive fibrosis. Similar changes were previously reported in animals with mechanically induced muscle strains. Unlike soft tissue sarcoma these lesions are small, non-progressive and associated with chronic quadriceps muscle strains. Most soft tissue tumors are not usually confined to the region of the tendon. Although on axial sections, both the muscle strain and the soft tissue tumor may have a similar appearance, sagital and coronal planes may demonstrate the longitudinal pattern of the strain. Without a clear history of trauma or infection, the presence of an unexplained soft tissue mass is a cause for concern. Ultrasound and MR imaging may help to differentiate a traumatic injury from a sarcoma. The radiologist should look for the diagnostic signs in different imaging techniques. However, in the absence of them, a biopsy of the lesion should be undertaken.
Differential Diagnosis List
Final Diagnosis
Rectus femoris muscle tear
Liscense
Figures
Ultrasound scans of the quadriceps muscle, axial views.


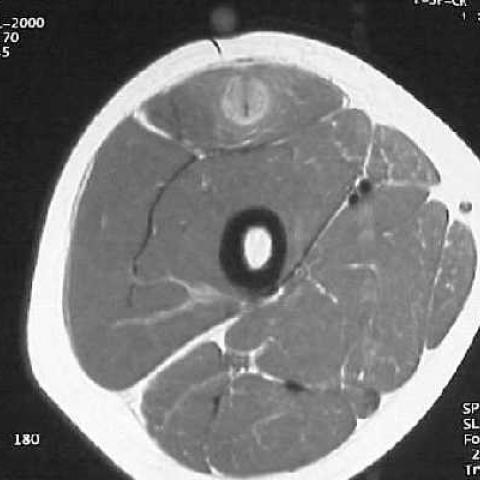
MRI of the quadriceps muscle.




I. Imaging Findings
1. Ultrasound findings:
• A soft tissue mass of approximately 3×8 cm is visible in the anterior portion of the quadriceps muscle (primarily the rectus femoris), appearing as a round or oval abnormal echoic area;
• In the transverse view, the periphery exhibits a "rim sign"; the mass shows heterogeneous echoes internally, with some areas revealing low-echo bands suggesting fluid accumulation or an old hematoma;
• Longitudinal and transverse scans reveal partial discontinuity or tearing of the tendon/muscle fibers, indicating possible fiber disruption along with a small amount of scar tissue or chronic inflammatory response.
2. MRI findings:
• On T2-weighted images, high signal abnormalities can be observed within the rectus femoris and around the tendon, partially presenting a ring-like or "target sign" appearance, with a slightly high signal surrounding a low signal band in the center;
• No clear evidence of bone involvement; the overall muscle structure remains relatively intact;
• The lesion is localized, with no obvious aggressive extension into surrounding soft tissue or bone structure;
• Post-contrast scans show enhancement of the muscle tissue and surrounding areas, consistent with chronic fibrosis or inflammatory changes.
3. Pathology:
• Biopsy results indicate localized chronic inflammation and reactive fibrosis;
• No neoplastic cell proliferation or signs of malignancy were observed.
II. Potential Diagnoses
- Chronic Rectus Femoris Tear or Stress Injury: Based on the “rim sign” on ultrasound and focal high signal on MRI suggesting an older tear with fibrotic repair, supported by pathology showing chronic inflammation and fibrosis.
- Soft Tissue Sarcoma: In cases of an unexplained soft tissue mass without a history of trauma, a tumor should be ruled out; however, imaging and pathology here support benign repair changes.
- Chronic Inflammation or Rare Inflammatory Myopathy: If muscle pain and a local mass appear, differential diagnoses also include localized infection or granuloma; yet no typical infection or granulomatous findings were noted histologically.
III. Final Diagnosis
Considering the patient’s age (7 years old), clinical presentation (mild thigh pain, no significant functional impairment), imaging findings (both ultrasound and MRI show chronic tearing with fibrotic changes), and histopathology (no malignant cells, indicating chronic inflammation and reactive fibrosis), the most likely diagnosis is:
“Chronic Rectus Femoris Tear with Reactive Fibrosis”
IV. Treatment Plan and Rehabilitation
1. Conservative Management:
• For pediatric patients with mild pain and no significant functional deficits, conservative treatment is preferred initially;
• This includes avoiding heavy loading and high-intensity activities that could cause reinjury;
• Symptomatic relief may be provided by mild anti-inflammatory and analgesic medications (e.g., NSAIDs).
2. Physical Therapy and Rehabilitation:
• Early Stage (Inflammatory Period ~2 weeks):
▪ Perform passive or assisted range-of-motion exercises within pain tolerance to maintain joint mobility;
▪ Low-intensity muscle strengthening, such as using resistance bands for isometric quadriceps contractions;
▪ Frequency: 2–3 times per week; Intensity: very low load; Time: 15–20 minutes each session; Type: joint mobility maintenance and isometric exercises;
▪ Monitor pain and swelling, gradually transitioning to the next phase.
• Intermediate Stage (Repair-Reconstruction ~2–6 weeks):
▪ Gradually introduce resisted quadriceps exercises, using light weights or bodyweight squats, straight leg raises, etc.;
▪ Incorporate moderate aerobic activities such as swimming or cycling to improve circulation and facilitate inflammatory resolution;
▪ Frequency: 3–4 times a week; Intensity: low to moderate, increasing with pain tolerance; Time: 20–30 minutes per session; Type: limited-range strength training and low-impact aerobic exercises;
▪ Gradually extend the duration of exercises.
• Late Stage (Functional Strengthening, after 6 weeks):
▪ In the absence of pain or with minimal discomfort, gradually increase muscle strengthening and joint flexibility exercises, e.g., moderate running or stationary jumping;
▪ Frequency: 3–5 times a week; Intensity: moderate load, progressively increased; Time: 30 minutes or more; Type: exercises targeting quadriceps strength and power;
▪ As the patient’s age and condition improve, training intensity and volume should be increased progressively (Progression principle).
3. Surgical Indication:
• Surgery may be considered for persistent and worsening pain or significant functional impairment, particularly if imaging shows extensive tendon disruption or poor scar healing;
• Postoperative rehabilitation protocols should be strictly followed to ensure gradual recovery of muscle strength and joint range of motion.
4. Precautions:
• In this case, the patient experiences only mild pain with no evident activity restriction, so a conservative approach and stepwise rehabilitation are typically sufficient;
• Monitor local responses and pain levels closely during rehabilitation, adjust exercise intensity accordingly;
• Parents should partner with physicians and physical therapists to foster compliance with the rehabilitation program, thereby avoiding recurrent injury or exacerbation.
Disclaimer:
This report provides a reference analysis based on available information and does not substitute for in-person consultation or professional medical advice. If symptoms persist or worsen, please seek medical evaluation for further assessment and individualized treatment recommendations.
Human Doctor Final Diagnosis
Rectus femoris muscle tear