Sonographic target sign in a case of benign neurofibroma



Clinical History
A soft tissue tumefaction located in the gluteal region in a patient affected by neurofibromatosis type 1 (NF1). The lesion presented a "target" pattern on both ultrasonography and MR imaging.
Imaging Findings
The patient presented with diagnosis of neurofibromatosis Type 1 (NF1), based on clinical parameters - a family history of NF1 and lots of light brown ("café-au-lait") spots on the skin. He underwent ultrasonography and MR evaluation of a soft tissue mass in the left gluteal region.
Ultrasonography, performed by a 7.5 MHz transducer, revealed a soft tissue mass measuring 5cm by 3 cm in size, localised along the course of the sciatic nerve. The lesion showed an oval shape with well-defined margins; the echostructure appeared relatively hypoechoic on the outer portion with a central region of increased echogenicity. Longitudinal and transverse scans were performed along the expected course of the sciatic nerve, but it could not be identified.
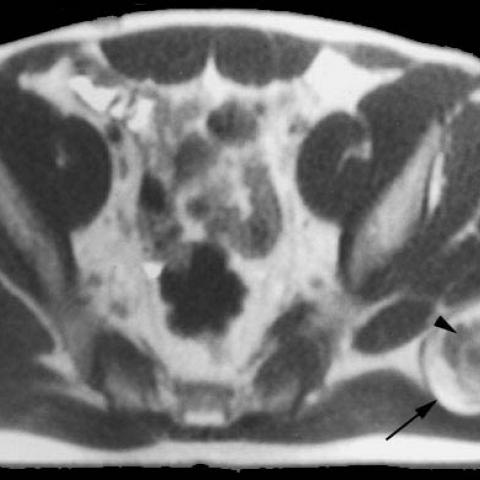
MRI was performed by a 0.2 T unit, on axial, sagittal and coronal planes, using SE T1- and T2-weighted, T1-STIR and T1-enhanced sequences. The lesion showed isointense signal with the surrounding muscular tissue, with a hypointense peripheral rim on T1-weighted sequences. It displayed high signal intensity on T2-weighted imaging with a hypointense central region and appeared strongly enhanced after i.v. gadolinium administration.
The patient underwent surgery and the histological specimen demonstrated a cellular mass composed of compactly packed neurofibroma cells and collagen surrounded by a less compact region containing an abundant myxoid stroma.
Discussion
Neurofibromas are the most common tumours of peripheral nerves [1]. Many authors have described a target pattern of neurofibroma on magnetic resonance studies of peripheral nerve tumours and found that the presence of the target pattern is more common in benign nerve sheath tumours. This can allow differential diagnosis with malignant peripheral nerve sheath tumor (MPNST) which often arises within an existing neurofibroma (in about 2% of NF1 patients) [2-3].
In previously reported MR imaging-histological correlation studies, the target sign reflects the mode of tumour formation - with dense fibrous and collagenous central zones corresponding to the low signal centre on T2-weighted images. Abundant myxoid material with high fluid content in the outer zones corresponds to the high signal periphery on T2-weighted images [3-5].
We believe that this case report is significant in describing the presence of the target pattern of the neurofibroma on both MR and ultrasonography images.
Differential Diagnosis List
Final Diagnosis
Benign neurofibroma
Liscense
Figures
Sonographic transverse scanning of the gluteal region

MR SE T2-weighted axial (a) and sagittal (b) scanning

MR SE T1-weighted axial scans before and after intravenous gadolinium


Medical Analysis Report
1. Imaging Findings
1) The patient is a 35-year-old male, already diagnosed with Neurofibromatosis Type 1 (NF1). The main clinical manifestation is a soft tissue mass in the right buttock.
2) Both ultrasound and MRI reveal a lesion showing a “target sign,” specifically:
• On ultrasound, the central area of the mass is relatively dense or shows lower echogenicity, while the peripheral area appears relatively hyperechoic;
• On T2-weighted MRI, there is reduced signal in the central region (indicating abundant fibrous or collagenous tissue) and increased signal in the peripheral region (indicating a myxoid stroma or higher water content);
3) The lesion typically has relatively clear margins with identifiable boundaries from the surrounding soft tissue. Currently, there is no obvious destruction of nearby bony structures or marked infiltration.
2. Potential Diagnoses
Based on the existing clinical history (NF1) and the imaging characteristics (especially the double “target sign”), the following diagnoses or differential diagnoses should be considered:
1) Neurofibroma: Common in patients with NF1. The classic MRI “target sign” often suggests a benign nerve sheath tumor;
2) Schwannoma: Also a peripheral nerve sheath tumor that can sometimes present similar findings, but neurofibromas are more frequently observed in NF1;
3) Malignant Peripheral Nerve Sheath Tumor (MPNST): In NF1 patients, there is some probability that a neurofibroma will undergo malignant transformation. On MRI, MPNSTs often appear larger, have irregular borders, show heterogeneous internal signals, and exhibit the “target sign” less commonly. They are often accompanied by progressive symptoms or invasive features;
4) Other soft tissue tumors (e.g., lipoma, fibroma) may exhibit certain similar features on ultrasound or MRI, but usually lack the classic “target sign” and do not have the NF1 background.
3. Final Diagnosis
Taking into account the patient’s age, underlying NF1, and the typical imaging presentation (target sign), the most likely diagnosis is: Neurofibroma.
If uncertainty remains regarding the nature of the lesion, histopathological examination (biopsy) can be performed for further confirmation. Close follow-up is advised for NF1 patients to monitor any potential malignant transformation.
4. Treatment Plan and Rehabilitation
1) Treatment Strategy
• Observation or Conservative Management: For mild symptoms, small tumor size, or slow-growing lesions, periodic follow-up is recommended to monitor tumor changes and assess functional impairment;
• Surgical Treatment: In cases of progressive enlargement, significant local pain, functional impact, or suspicion of malignancy, early surgical excision is advised;
• Adjuvant Therapy: If pathological findings indicate malignancy, combined modalities such as radiation and chemotherapy may be considered; however, conventional radiation and chemotherapy are generally not applied to benign neurofibromas.
2) Rehabilitation/Exercise Prescription
Because this condition primarily involves soft tissue tumors, if there is no severe pain or neurological deficit, the exercise prescription should focus on maintaining or improving function in the lower limbs, trunk, and hip region. Progress gradually and tailor the plan to the individual, applying the FITT-VP principle (Frequency, Intensity, Time, Type, Volume, Progression). A sample approach is as follows:
• Early Stage (Preoperative or Conservative Observation Period)
- Frequency: 3–4 sessions per week, with at least 1 day of rest between sessions;
- Intensity: Moderate or low intensity, avoiding heavy-impact actions or high-load squats;
- Time: 20–30 minutes per session, possibly divided into several sets;
- Type: Includes low-resistance core muscle training (e.g., seated or standing leg raise, bridge exercise), range-of-motion activities (e.g., lumbar extensions), and moderate aerobic exercises (e.g., walking, elliptical);
- Monitoring: Exercise in a pain-free or mildly sore range. If there is significant local pain or noticeable tumor enlargement, seek medical evaluation promptly.
• Mid-to-Late Stage (Postoperative or Rehabilitation Phase)
- Adjust training intensity and duration according to the surgical outcome and lesion site. Gradually introduce light resistance exercises (e.g., resistance bands, dumbbells) and stability training (e.g., single-leg balance);
- Increase frequency to 4–5 times per week, each session lasting 30–40 minutes;
- Continue to monitor local healing and pain. If discomfort or functional impairment occurs, consult a rehabilitation specialist or physician to modify the plan.
Disclaimer:
This report is based solely on available information and serves as a reference for analysis. Please adhere to in-person medical consultations and follow the advice of qualified medical professionals for diagnosis and treatment. Any treatment or rehabilitation plan must be individualized and carried out under professional guidance.
Human Doctor Final Diagnosis
Benign neurofibroma