Plexiform neurofibroma of the ankle: evaluation with US and MRI



Clinical History
A case of a large soft tissue mass of the ankle in a patient affected by NF1.
Imaging Findings
The patient, who was affected with neurofibromatosis type 1, was referred for the pre-operative staging of a large tumefaction in the left ankle. The diagnosis of plexiform neurofibroma had been substantiated by prior surgical procedures, but none of these provided long-term resolution of the problem.
The patient complained of sharp pain, exacerbated by walking, at the posterior and medial side of the left ankle. A soft tissue mass, extending approximately 8 to 10 cm was palpable. A positive Tinel's sign was also present, indicating involvement of the tibial nerve.
The patient underwent ultrasonography (US) and magnetic resonance imaging (MRI) of the left ankle. US, performed with a 7.5-10 MHz transducer, revealed in the medial and posterior side of the ankle a dishomogeneous, widely extending, unclearly defined, tissue mass, which enveloped nearby soft tissues, vessels and tendons (Fig. 1). Longitudinal and transverse scans performed along the side of the posterior tibial nerve showed a fusiform swelling of the nerve which indicated the origin of the neurofibroma (Fig. 2).
MRI was performed with a 1.5 T unit, on axial, sagittal and coronal planes, using SE T1-, T1- fat-suppression, before and after i.v. gadolinium administration, and T2-weighted sequences. MRI showed higher resolution on the local extension of the mass with better visualisation of soft tissue and tendon involvement. The lesion’s signal intensity appeared iso–hypointense on T1–weighted sequences (Fig. 3a); high and dishomogeneous on T2–weighted sequences (Fig. 3c); and after i.v. gadolinium administration, marked and dishomogeneous enhancement with a multistratified pattern was seen (Fig. 3b).
The patient underwent another surgical excision, but a complete resection was impossible because of the large size of the lesion and the fact that it enveloped tendons, vessels and nerves. However, the surgical result is excellent cosmetically and in terms of pain relief.
Discussion
Neurofibromatosis, also known as von Recklinghausen's disease, is a phakomatosis that displays a wide spectrum of clinical expression with neurocutaneous abnormalities and involvement of multiple organ systems [1]. The hallmark of von Recklinghausen's disease is the neurofibroma. Neurofibromas in NF1 can be divided into three types: localised, diffuse or even large plexiform masses. Localised neurofibroma is the most common type seen with NF1. However, both localised and diffuse neurofibromas occur also in patients who are not affected by NF1 [2].
Plexiform neurofibroma is pathognomonic of NF1, and its development usually occurs in early childhood and precedes cutaneous neurofibromas. Pathologically, a plexiform neurofibroma represents diffuse involvement of a long nerve segment and its branches with tortuous expansion, and its gross appearance has been described as a "bag of worms". Because of its large size, this lesion commonly extends beyond the epineurium into the surrounding tissue. Plexiform neurofibroma may be associated with massive and disfiguring enlargement of an extremity, called elephantiasis neuromatosa [2]. Neurofibromas are intimately associated with the parent nerve, growing in a longitudinal fusiform manner, with the nerve "entering and exiting" from the lesion without being encapsulated.
Integrated imaging by US and MRI is useful in the diagnosis and preoperative staging of plexiform neurofibromas. Sonography shows a dishomogeneous, hypoechoic, widely extending lesion, unclearly defined, which envelops the surronding soft tissues [2-5]. US is the first step; MRI is better at determinating the extent of the lesion and involvement of contiguous structures, therefore permitting an accurate preoperative staging. MRI reveals low-signal-intensity lesions on T1-weighted sequences, high-signal-intensity lesions on T2-weighted sequences, and avid contrast enhancement [2-5]. Another typical feature is a fusiform shape, oriented longitudinally along the nerve distribution, often revealing tapered ends which are contiguous to the parent nerves.
Surgical resection requires sacrificing of the parent nerve because the neurofibroma cannot be separated from the nerve fibres. Attempts at surgical resection are usually reserved for markedly symptomatic lesions that substantially compromise function. Because of its large size, surgical resection of the lesion is often incomplete, leading to frequent recurrences. Malignant transformation to malignant PNST is the most feared complication of NF1. The estimated prevalence of malignant transformation varies from 2% to 29%, with an average of approximately 5% [1-2].
Differential Diagnosis List
Final Diagnosis
Plexiform neurofibroma
Liscense
Figures
Ultrasonography of the ankle
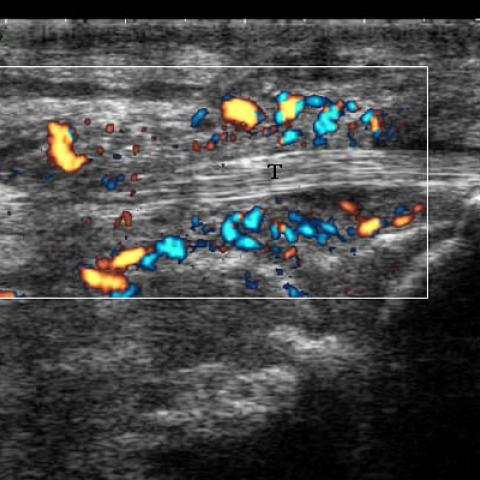

Ultrasonography of the ankle

Magnetic resonance imaging of the ankle



Medical Imaging Analysis Report
I. Imaging Findings
Based on ultrasound and MRI examination results, the main observations are as follows:
- Overall Position and Extent: A large soft tissue mass is visible in the ankle region, involving the surrounding soft tissues.
- Ultrasound (Color Doppler) Findings:
- The lesion shows heterogeneous hypoechoic areas with unclear boundaries, encasing surrounding structures.
- Color Doppler indicates varying degrees of blood flow, suggesting a relatively rich blood supply.
- The lesion exhibits extensive extension along the course of the nerve.
- MRI Findings:
- On T1-weighted images, the lesion appears as a low signal area.
- On T2-weighted images, the lesion appears as a high signal area with uneven signal intensity, showing obvious enhancement after contrast administration.
- A characteristic spindle-shaped or “bag-like” morphology can be observed, with its long axis consistent with the direction of nerve distribution.
- There is varying degrees of soft tissue infiltration, with poorly defined borders.
II. Potential Diagnosis
Combining the imaging findings and clinical history (Neurofibromatosis Type 1, NF1), the following diagnoses or differential diagnoses are considered:
- Plexiform Neurofibroma: Highly characteristic in NF1, often presenting as a “bag-like” lesion with diffuse longitudinal thickening along the nerve. The MRI findings in this case are consistent with this pattern.
- Schwannoma: Another benign neoplasm arising from the nerve sheath, which can exhibit enhancement but often appears as a relatively well-defined elliptical lesion or with a target-like appearance. Its growth pattern generally differs from the “plexiform” form associated with NF1.
- Malignant Peripheral Nerve Sheath Tumor (MPNST): Patients with NF1 have an increased risk of malignant transformation, which often appears more aggressive on imaging with possible local bone destruction or more pronounced soft tissue infiltration.
III. Final Diagnosis
Based on the patient’s confirmed history of NF1, the characteristic imaging findings (low signal on T1, high signal on T2, alignment with nerve distribution, and “bag-like” appearance), and the clinical presentation, the most likely diagnosis is:
Plexiform Neurofibroma.
If there are signs suggesting malignant transformation or a progressive worsening of symptoms, a biopsy can be considered to further clarify the nature of the lesion.
IV. Treatment Plan and Rehabilitation
Common treatment strategies and rehabilitation recommendations for plexiform neurofibroma are as follows:
- Treatment Strategies:
- If the lesion is large and affects function or causes pain, surgical resection may be considered. However, because plexiform neurofibromas are often closely intertwined with nerve fibers, complete resection usually requires sacrificing part of the nerve, potentially resulting in related nerve function deficits.
- For patients with mild symptoms that do not significantly affect function or appearance, regular follow-up and observation are recommended, monitoring for any malignant changes.
- Suspected malignant transformation or rapidly progressing clinical manifestations may warrant more aggressive surgical intervention and adjunctive therapy as early as possible.
- Rehabilitation and Exercise Prescription:
- Perform individualized rehabilitation exercises under the guidance of a physician or rehabilitation therapist to protect the affected limb and gradually improve ankle and lower limb muscle strength and joint range of motion.
- Initially, adopt low-intensity, short-duration exercises with gradual progression, such as:
- Range-of-motion exercises: In the absence of pain, perform ankle flexion, extension, and circular movements for 5–10 minutes each session, 2–3 times a day.
- Light weight-bearing exercises with support: For example, walking with assistive devices or crutches to ensure a stable gait.
- As the condition and tolerance improve, gradually increase the intensity and duration of the exercises (following the FITT-VP principle), for instance:
- Extend each exercise session to 15–20 minutes and include mild resistance training or elastic band exercises.
- Incorporate muscle strengthening exercises such as toe raises and ankle stability workouts 3–4 times a week.
- Throughout the rehabilitation process, avoid excessive weight-bearing or high-impact activities. Pay close attention to any potential nerve dysfunction or muscle weakness in the affected limb to prevent falls or further injury.
V. Disclaimer
This report is based on the current medical history and imaging data for reference purposes only and does not replace in-person medical consultation or professional medical advice. The patient should follow the instructions of specialized medical professionals for subsequent diagnosis, treatment, and rehabilitation.
Human Doctor Final Diagnosis
Plexiform neurofibroma