Accessory soleus muscle



Clinical History
A 16-year-old female, classical ballet dancer, presented to us with a long history of pain in her right ankle.
Imaging Findings
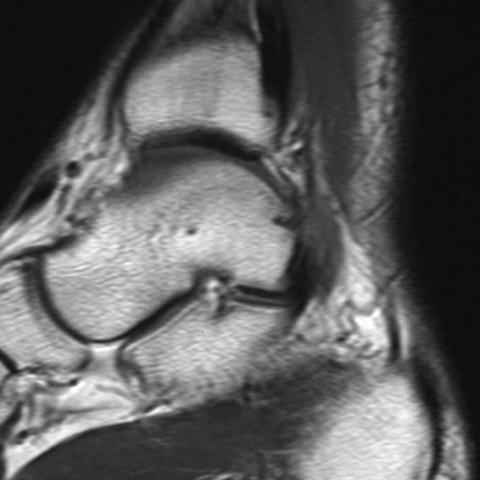
A 16-year-old female classical ballet dancer presented to us with a long history of pain in her right ankle. She had no past history of trauma of the affected ankle. A radiographic examination when done gave normal results and an MRI was carried out to further explain the symptoms. Axial and sagittal T1-weighted MR images that were obtained revealed abnormal muscle tissue, obscuring the fat in Kager’s triangle. On the basis of clinical and MRI findings, accessory soleus muscle was diagnosed. Neither surgery nor a biopsy was performed.
Discussion
The accessory soleus muscle is a rare (8%) and a usually incidental MRI Finding. However, in some cases, it can be responsible for a posterior ankle impingement syndrome with posterior pain, focal edema and varus deformation. It occurs more often in athletes in whom there is a tendency of accessory soleus hypertrophy. The upper origin of the muscle is the soleus aponeurosis or the posterior face of the tibia diaphysis. The muscle belly is medial, and is separated from the soleus muscle by its own aponeurosis. Several insertions which have been described are: into the calcaneal tendon, into the upper face, medial face or both faces of the calcaneus. The accessory soleus muscle can be diagnosed using sonography, Computed tomography and, more reliably, MRI based on location and signal characteristics. Axial and sagittal T1- and T2-weighted MR images of the ankle may reveal a fusiform mass filling Kager’s triangle. This mass appears isointense when compared with other muscles in T1- and T2-weighted images but is more clearly seen in T1-weighted images because of the high intensity of the fat surrounding it within Kager’s triangle. Sagittal T1-weighted MR images also show the hypointensity of the accessory soleus tendon and the type of insertion. In some cases, clinical complaints may indicate the need for surgical excision.
Differential Diagnosis List
Final Diagnosis
Accessory soleus muscle.
Liscense
Figures
Accessory soleus muscle


1. Imaging Findings
Based on the provided ankle MRI images, a spindle-shaped abnormal soft tissue shadow is observed posterior to the right ankle in the Kager’s triangle region. The signal of this soft tissue is approximately isointense to the surrounding normal muscle tissue on both T1 and T2 weighted images. However, due to the significantly high signal intensity of the surrounding adipose tissue, this mass is more readily identifiable on T1 weighted images.
The muscle belly courses slightly medially, with a clear boundary from the normal soleus muscle, suggesting that it may independently originate from the posterior tendon sheath or the posterior surface of the tibia, and possess an independent attachment near the calcaneus or Achilles tendon. There are no obvious signs of bone destruction, no evident bone marrow edema, or ligament rupture in the surrounding tissues. Mild edema or signs of inflammation can be seen within the soft tissue.
2. Potential Diagnoses
- Accessory Soleus Muscle: Based on the imaging features, the patient’s age, and ballet training history, an abnormal muscle mass attached to the calcaneus or Achilles tendon is most likely an accessory soleus muscle. It can lead to posterior ankle pain and impingement syndrome, especially apparent during weight-bearing or dance movements.
- Other Posterior Ankle Soft Tissue Lesions (such as soft tissue tumors or synovial cysts): For example, giant cell tumors, lipomas, or rare synovial cysts. However, these lesions typically present signal characteristics on T1 and T2 weighted images that differ from muscle (e.g., lipomas typically show high signal on T1 images).
- Paratenonitis or Tenosynovial Lesions: Primarily related to Achilles tendon or soleus tendon inflammation. However, the anatomical structure and signal seen on imaging are consistent with an independent muscle, making this less likely.
Given that the patient is a classical ballet dancer, experiencing repeated overextension and load on the posterior ankle, and that the MRI shows a soft tissue signal consistent with muscle tissue, the most likely diagnosis is an accessory soleus muscle.
3. Final Diagnosis
Combining the patient’s clinical symptoms (persistent right ankle pain and a background in dance) with the MRI findings, the most likely diagnosis is:
Accessory Soleus Muscle Causing Posterior Ankle Impingement Syndrome
If symptoms persist and are accompanied by joint dysfunction, further confirmation can be obtained via physical examination, histopathological evaluation, or additional diagnostic methods.
4. Treatment Plan and Rehabilitation
Treatment strategies can be tailored according to the severity of the patient’s symptoms and functional needs:
- Conservative Treatment:
- Temporarily reduce or avoid activities that cause excessive compression in the posterior ankle (e.g., standing on tiptoe or maximal plantar flexion).
- Use an ankle brace or heel lift to lessen impact on the posterior ankle region.
- Short-term use of oral anti-inflammatory and analgesic medications (e.g., NSAIDs) for pain relief.
- Physical therapy and rehabilitation: Local treatments such as heat therapy, ultrasound, or low-frequency electrical stimulation can help reduce muscle tension and inflammation.
- Surgical Treatment:
- If significant posterior ankle impingement symptoms or notable muscle hypertrophy impacts dance performance or quality of life, surgical removal of the accessory soleus muscle may be considered to relieve symptoms.
Exercise Prescription & Rehabilitation Highlights (Using the FITT-VP Principle):
- Frequency: At least 3–4 rehabilitation sessions per week.
- Intensity: Start within a pain-free range at mild intensity, gradually progressing to moderate intensity. If the pain scale exceeds 4 out of 10, reduce intensity accordingly.
- Time: Each session should last 20–30 minutes, including warm-up and stretching.
- Type:
- Low-impact activities such as swimming or cycling can be used for cardiovascular and foundational lower limb strength training.
- Ankle stability and small muscle group strengthening exercises, including balance board training and resistance band exercises.
- Volume & Progression: As pain decreases and ankle stability improves, gradually increase tiptoe maneuvers, half squats, and jumping exercises in terms of frequency and sets. Adhere to a pain-free or low-pain principle throughout.
Note: Since the patient is still in a growth and development stage, care should be taken to avoid overtraining that might cause soft tissue or growth plate injuries. Under the guidance of a specialist physician or athletic trainer, gradually increase the load to prevent recurrence and long-term complications.
Disclaimer: This report is based solely on current imaging and the patient’s history for preliminary analysis and does not replace an in-person diagnosis or the final opinion of a professional healthcare provider. For confirmation of the condition and implementation of a treatment plan, please consult a specialist in a certified medical institution.
Human Doctor Final Diagnosis
Accessory soleus muscle.