Avascular Necrosis of the Hip in a Teenager



Clinical History
This patient, born in the Congo, was diagnosed with sickle cell disease aged 9 months. An MRI showed avascular necrosis (AVN) of the left hip. We present a series of plain radiographs and an MRI demonstrating the development and treatment of AVN of the hip due to sickle cell disease.
Imaging Findings
The patient presented complaining of increasing left hip pain for several weeks. He had a background history of sickle cell disease. There is no family history of hip pathology. Examination of the painful hip revealed a decrease in internal rotation and spasms at the extremes of all planes of motion. Plain radiographs suggested a diagnosis of an osteochondral fracture with epiphyseal involvement. The patient was admitted for treatment with skin traction pending a bone scan and MRI scan. The MRI and bone scan diagnosed AVN of the left hip and splenomegaly. The patient was discharged home partial weight bearing on crutches. Eight months later he was readmitted via outpatient clinic with a two week long history of worsening limp and increasing left hip pain. Examination again demonstrated decreased hip movements: flexion =120 degrees, internal rotation = 0 degrees, external rotation = 30 degrees and abduction = 40 degrees. He was treated with skin traction effectively and discharged 24 hours later nonweight bearing, with a planned admission date for an arthrogram. This was performed as a day case and showed significant hinge abduction of the left hip. This was treated six weeks later with a proximal femoral valgus osteotomy, psoas and adductor release. Post operatively the patient was managed with traction and a single hip spica. He was discharged nonweight bearing. We plan to remove the screws at a subsequent date.
Discussion
Sickle cell disease is an autosomal recessive chronic haemoglobinopathy. In sickle cell disease, aseptic skeletal conditions have two causes: chronic haemolytic anaemia leading to marrow hyperplasia and hypoxia leading to red cell sickling ischamia and infarction. 1 In adolescence and adulthood, a common complication of sickle cell disease is AVN typically in areas supplied by end arteries such as the femoral or humeral heads. Patients often have pain associated with functional limitation of the affected joint. Chronic pain is often associated with later stages of AVN necrosis, particularly in the femoral head. Weight bearing on the joint exacerbates the pain due to AVN. Infarction of bone and bone marrow in patients with sickle cell disease can lead to the following radiological changes: • osteolysis (in acute infarction) • AVN • articular disintegration • myelosclerosis • periosteal reaction (unusual in the adult) • H vertebrae (step like depression in the end plates)4 Areas of AVN become radiographically visible as sclerosis of bone with secondary repair reaction and eventually result in degenerative bone and joint destruction. In a UK study in 1991 a series of 41 patients with sickle cell disease eleven (41%) were affected by AVN of the femoral head. Seven (26%) had bilateral disease.2MRI is the best method for detecting early signs of AVN in patients with sickle cell disease and for identifying episodes of osteomyelitis. Nuclear scanning can also be used to detect early AVN. Plain radiography is useful in evaluating subacute and chronic infarction but is of little value in the acute phase of AVN where MRI has little advantage.3Perthes’ disease normally affects younger children. In older children and adolescents a Perthes ‘lesion’ probably is equivalent to idiopathic AVN.
Differential Diagnosis List
Final Diagnosis
Left hip AVN, secondary to sickle cell disease.
Liscense
Figures
Fig 1. Radiograph on initial presentation

Fig 2. Radiograph 1 months after presentation.

Fig 3. Radiograph 3 months after presentation

Fig 4. Pre operative, 9 months after presentation.

Fig 5. Post operative proximal femoral valgus osteotomy radiograph.
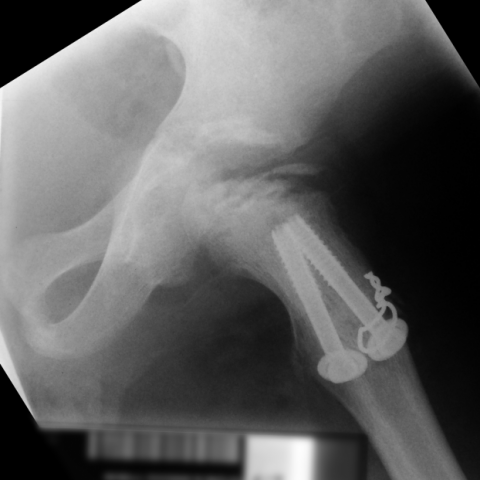
Fig 6. MRI scan. Coronal STIR sequence: Extensive signal abnormality is seen in the left femoral head.The central column of the femoral head returns abnormal low signal and heterogenous signal is seen arising from the femoral neck. There is a small joint effusion but no synovial thickening. There is cortical thickening along the medial aspect of the femoral neck with a suggestion of periosteal lifting consistent with a previous insult. The right femoral head is flattened and broadened although signal return is more normal, reflecting previous avascular necrosis.

Medical Imaging Analysis Report
1. Imaging Findings
Based on the provided anteroposterior (AP) radiograph of the hip joint and MRI images, abnormal structural changes can be observed in the left femoral head. The main observations include:
- Abnormal femoral head morphology: Some radiographs show mild collapse or flattening of the left femoral head contour, along with findings suggestive of sclerosis.
- Changes in density: Localized sclerotic bands and radiolucent areas are apparent, indicating the coexistence of necrotic bone and reparative response.
- Joint space: A certain degree of joint space change is still observed. In some cases, subchondral fractures or bone collapse may occur, but detailed assessment should be performed using multi-angle imaging.
- MRI signals: On T1- and T2-weighted images of the left femoral head, signal changes can be seen, suggesting avascular areas and bone marrow edema. A characteristic abnormal signal band helps in the early diagnosis of femoral head necrosis.
Overall imaging characteristics are consistent with avascular necrosis (AVN) of the femoral head, especially in the setting of a previously confirmed diagnosis of sickle cell disease (SCD).
2. Potential Diagnoses
Based on the patient’s clinical information (13-year-old male with a lifelong history of sickle cell disease) and the imaging findings described above, the following potential diagnoses are considered:
- Avascular Necrosis (AVN) of the Femoral Head:
- Sickle cell disease is a common cause of femoral head AVN due to sickling of red blood cells and disrupted blood flow, leading to inadequate local blood supply.
- Imaging findings may include collapse of the femoral head, density abnormalities, sclerotic bands, and classic subchondral fracture lines.
- Epiphyseal Osteonecrosis (e.g., Legg-Calvé-Perthes Disease):
- Commonly seen in children aged 4–10. If imaging findings resemble AVN, further differentiation may be necessary.
- In this case, the patient is older (13 years) and has a known underlying condition (sickle cell disease). Perthes disease is less likely, and the usual clinical course and presentation differ.
- Osteomyelitis or Infectious Lesions:
- Patients with sickle cell disease are prone to osteomyelitis, which can sometimes present with imaging findings similar to bone necrosis.
- However, MRI can usually distinguish infection from aseptic necrosis, and clinical symptoms also differ.
Considering the patient’s history, sickle cell disease–induced aseptic necrosis of the femoral head remains the most likely diagnosis.
3. Final Diagnosis
Taking into account the patient’s age, medical history (sickle cell disease diagnosed in early childhood), clinical symptoms (hip pain, restricted mobility), and imaging findings (femoral head collapse, sclerosis, and MRI signal changes), the most probable diagnosis is:
Left Femoral Head Avascular Necrosis (AVN) Secondary to Sickle Cell Disease.
If any doubts remain or if further evaluation of lesion activity and extent of subchondral fractures is needed, higher-resolution MRI sequences or additional imaging and laboratory tests should be considered to rule out infection or other complications.
4. Treatment and Rehabilitation Plan
The following treatment strategies may be selected in consultation with the medical team, based on the patient’s specific situation:
- Conservative Management:
- Weight-bearing restriction: Use of crutches or a walker to reduce sustained pressure on the affected hip.
- Pain relief and anti-inflammatory therapy: Oral NSAIDs or other pain medications to alleviate discomfort.
- Close monitoring: Regular imaging follow-up to observe the extent of femoral head necrosis and degree of collapse.
- Surgical Management:
- Core Decompression: Suitable at early stages to decrease intramedullary pressure and promote new blood vessel formation.
- Vascularized Bone Grafting: An option if necessary to enhance local repair.
- Joint Reconstruction Surgery: In cases of significant collapse, arthritic changes, or severe functional impairment, hip replacement surgery may be considered.
- Rehabilitation and Exercise Prescription:
- Early Rehabilitation: During acute phases or immediately post-surgery, non-weight-bearing or partial weight-bearing activities can be performed, such as active or passive range-of-motion exercises in seated or supine positions, to maintain joint mobility and prevent muscle atrophy.
- Gradual Increase in Exercise Intensity: Following the FITT-VP principle (Frequency, Intensity, Time, Type, Progression, Volume), activity levels are gradually raised. For example:
- Frequency: 3–4 times per week, with appropriate rest intervals.
- Intensity: Start with low intensity to avoid significant pain (e.g., light resistance training with elastic bands).
- Time: Initially 10–15 minutes per session, gradually extended to 30 minutes.
- Type: Begin with static muscle strengthening, such as isometric quadriceps exercises, followed by moderate weight-bearing and gait training.
- Progression: Adjust resistance and duration gradually, depending on patient tolerance and clinical improvement.
- Safety Considerations: Avoid high-impact exercises; closely monitor hip pain and swelling. If severe symptoms occur, seek medical assessment promptly.
Individualized Approach
Throughout the rehabilitation process, exercise prescriptions should be tailored according to the patient’s skeletal condition, level of pain, and cardiopulmonary tolerance. Close collaboration with specialist physicians and rehabilitation therapists is crucial to maximize recovery and minimize the risk of complications.
Disclaimer: This report is a reference-based medical analysis and does not replace an in-person consultation or professional medical advice. Patients should undergo further evaluation and treatment under the guidance of specialist physicians and a dedicated medical team.
Human Doctor Final Diagnosis
Left hip AVN, secondary to sickle cell disease.