Neuropathic osteoarthropathy secondary to syringomielia


Clinical History
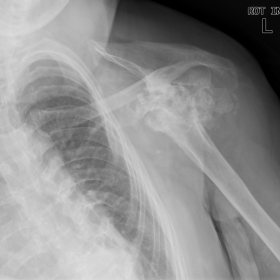
Patient with personal history of syringomielia, is referred to the clinician with swollen and warmth shoulders. AP radiographs of the left shoulder showed destruction of the humeral head and of the glenoid, with dislocation, marked productive changes and detachment of bone fragments.
Imaging Findings
A 63 year old female patient, tetraparetic, with past history of cervical laminectomy and drainage of syringomielic cavity, presented with a long history of edema, warmth and moderate pain in the shoulders. There where mild painful symptoms in the elbows, wrists and hands. AP radiographs of the shoulders revealed marked destruction of the left glenohumeral joint, with debris, joint distention and dislocation (fig. 1). The right shoulder showed intense osteoarthritis-like alterations, with exuberant osteophytes in the humeral head and bone debris (fig. 2). One can appreciate similar alterations in the left elbow (fig. 3). In the hands, bilateral degenerative alterations in the 3rd, 4th and 5th IFP articulations, sparing the 1st carpometacarpal and the IFD articulations, is amenable with neuropathic arthropathy (fig. 4). The articulations of the lower limb showed no significant alterations (fig. 5). There was paralytic kiphoscoliosis in the dorsal spine.
Discussion
The loss of sensory nervous function on musculoskeletal system results in severe joint damage. The joints, without sensitive feedback, are subjected to recurrent injury, leading to specific radiographic abnormalities wich are termed Neuropathic Osteoarthropathy or Charcot´s joint, since was French scientist Jean-Martin Charcot who first described this disease, in 1868 (1). The site of involvement in neuropathic osteoarthropathy depends of the etiology. In tabes dorsalis, the spine and the major articulations of the lower limb are affected. In syringomyelia the alterations are present in the glenohumeral joint, elbow, wrist and spine. Meningomyelocele involves ankle and intertarsal joints. In amyloidosis the knee and ankle are commonly affected. Diabetes mellitus and alcoholism show typical alterations in metatarsophalangeal, tarsometatarsal and intertarsal joints (2). The classic resulting radiographic picture of Charcot's joints is that of the "5 Ds": normal density, joint distention, bony debris, joint disorganization and dislocation. But almost 40% of neuropathic joint disease are atrophic, with severe bone resorption and little or no debris. The atrophic manifestation is more common in the upper extremities (3). Early manifestations of may simulate osteoarthritis and calcium pyrophosphate dihydrate crystal deposition disease. As the alterations evolve, Charcot's joints tend to exhibit large effusions, which may decompress along soft tissue planes and carry bony debris far from the joint. Bone resorption and formation occurs simultaneously. Bone eburnation, ligamentous laxity and subluxation are also evident. Ankylosis is rare. Neuropathic joint's may suffer infectious complications, particularly in diabetes mellitus (1). Syringomielia is the major cause of neuropathic shoulder. There may be also alterations in the elbow, wrist and fingers joints. Changes in the spine are most characteristic in the cervical region (1,3).
Differential Diagnosis List
Final Diagnosis
Neuropathic osteoarthropathy
Liscense
Figures
AP radiograph of the left shoulder

AP radiograph of the right shoulder

AP and lateral radiographs of the left elbow

AP radiograph of the hands

Articulations of the lower limb

Imaging Findings
The patient is a 63-year-old female with a history of syringomyelia. The current X-ray shows significant destruction of the humeral head and the glenoid rim in the left shoulder joint, with disorganized joint surfaces and evidence of dislocation. There are also signs of bony overgrowth and free bone fragments in the region. Imaging of other joints (including the elbow and wrist) reveals certain proliferative or destructive changes, possibly indicating the same or a similar pathological process (neuropathic joint damage).
Potential Diagnoses
Based on the patient’s imaging features and past medical history, the following differential or potential diagnoses should be considered:
- Neuropathic Arthropathy (Charcot Joint):
● The patient’s syringomyelia history often involves shoulder, elbow, and wrist joints.
● Imaging may show joint destruction, dislocation, bony overgrowth, and fragments, consistent with typical “5D” or atrophic-type characteristics.
● Clinically, there is frequently a loss of sensation with repeated injury leading to severe structural damage. - Erosive Osteoarthritis (Severe Osteoarthritis):
● May lead to local bony overgrowth, joint space narrowing, and cartilage destruction, but typically does not exhibit such extensive debris, dislocation, or the absence of protective neurological feedback. - Crystal-induced Arthropathy (e.g., CPPD):
● Some patients may demonstrate chondrocalcinosis and recurrent joint destruction; however, it is challenging to account for the marked bone destruction and dislocation seen here based on this alone. - Infectious Arthritis:
● Can cause bone destruction and changes in joint structure, but is usually accompanied by acute inflammatory responses and abnormal laboratory findings. Unless there is a coexisting infection, it is not the top differential diagnosis in this case.
Final Diagnosis
Taking into account the patient’s history of syringomyelia, the severe destructive and dislocative changes in the shoulder joint seen on imaging, and the characteristic hallmark of catastrophic joint destruction with fragmentation typical of neuropathic involvement, the most likely diagnosis is:
Neuropathic Arthropathy (Charcot Joint) secondary to Syringomyelia.
Treatment Plan and Rehabilitation Strategy
Given the features of neuropathic arthropathy, a comprehensive management approach should include:
- Underlying Cause Management and Monitoring:
● Proactively evaluate and manage the progression of syringomyelia; collaborate with neurology or spine surgery as needed to slow or stabilize neurological deterioration.
● Conduct regular follow-up of neurological function to prevent or detect potential complications early. - Joint Stabilization and Protection:
● Use protective braces or splints to reduce further joint damage.
● Provide adequate support to the shoulder or other affected joints, avoiding excessive weight-bearing or large range-of-motion movements. - Pain and Inflammation Control:
● Although neuropathic arthropathy may present with atypical pain due to sensory deficits, if secondary inflammation or pain exists, consider NSAIDs or other analgesics.
● If infection is suspected, actively initiate anti-infective treatment. - Surgical Intervention:
● In cases of severe deformities, persistent instability, or functional limitations, joint arthroplasty or fusion may be considered, with comprehensive assessment of the patient’s overall condition and neurological status.
● The aim of surgery is to stabilize the joint, reduce pain, and improve daily activity. - Rehabilitation and Exercise Prescription:
● Goal: To preserve or recover joint range of motion and muscle strength while protecting the joints, and to prevent disuse atrophy.
● Initial Phase: Start with gentle range-of-motion exercises, such as non-weight-bearing swing movements or passive movements, 1–2 sessions per day, approximately 10 minutes each.
● Progressive Phase: Once joint stability and pain are adequately managed, gradually introduce active range-of-motion exercises and mild resistance training (e.g., using resistance bands). Increase frequency to 3–4 sessions per week while monitoring for discomfort or local inflammation.
● Advanced Phase: If the joint condition allows, cautiously resume daily functional activities and postural training, potentially incorporating aquatic therapy or light-weight upper limb exercises.
● Important Considerations: Due to altered sensory and pain feedback, special vigilance is required to avoid overexertion or posture-related injuries to joints and soft tissues. Always inspect the skin and joints before and after exercise.
● FITT-VP Principle: Individualize frequency (3–4 times per week), intensity (mild resistance), time (10–20 minutes), type (range-of-motion and low-load strength training), volume (increased as tolerated), and progression (gradual increments).
Disclaimer:
This report provides reference-based analysis drawing on imaging findings and the available medical history; it does not replace in-person consultation or a professional medical opinion. Specific treatments should be determined by integrating the patient’s clinical presentation, laboratory findings, and other diagnostic results, in collaboration with a professional healthcare team.
Human Doctor Final Diagnosis
Neuropathic osteoarthropathy